Designing Behaviorally Informed Health Interventions: Adherence to Micronutrient Treatment in El Salvador

Context
In the poorest municipalities of El Salvador, anemia affects one out of two children under the age of two. If untreated, anemia can diminish cognitive functions, increase the risk of infections, and over the long-term cause permanent losses in productive capacity. In 2014 through the Salud Mesoamerica Initiative (SMI), dietary supplements (in the form of micronutrient powders) were introduced in the country as a preventive treatment for anemia in children. The first stage of the micronutrient intervention ended in 2015, and took a traditional approach that focused on the distribution of the micronutrient treatment. While this approach was effective in ensuring that children in the target area received the micronutrients (64 percent), only 15 percent consumed the full recommended regimen of 60 packets for 60 days every six months.
The Project
Building on the previous stage, the intervention was redesigned in 2016. To help track adherence to treatment, the intervention developed tools and strategies for community health workers and caregivers. It also added home visits by community health workers to provide caregivers encouragement and counseling and to monitor adherence. In addition, it gave caregivers a calendar so they could track their children’s progress over the course of the treatment.
Behavioral Analysis
Behavioral Barriers
Salience: Individuals tend to focus on items or information that are more prominent and ignore those that are less so. Thus, it is important to make key aspects of messages visible and salient and display them in an appropriate place and time. In this context, caregivers might be not fully aware of the potential problems and threats related to anemia. This is plausible because symptoms of anemia can easily go unnoticed.
Optimism bias: This behavior leads us to underestimate the probability that negative events will happen to us and to overestimate the probability of positive events. Since caregivers cannot perceive the symptoms of anemia until it the condition is diagnosed, they believe that the probability of their children getting sick is lower than it actually is.
Cognitive overload: The cognitive load is the amount of mental effort and memory used at a given moment in time. ‘Overload’ occurs when the volume of information presented exceeds an individual’s capacity to process it. Thus, the fact that our attention and memory are limited prevents us from processing all available information at the same time. Caregivers might be aware of the consequences of untreated anemia, but they might not have a clear understanding of how to avoid the preventable illness.
Hassle factors: Seemingly small inconveniences, such as having to read a lot of information or take an extra small step to complete an action, can hinder or disrupt decision-making processes. Children might not like the taste of the micronutrients or might not want to take them at all. In such situations, it is possible that caregivers would try just a few times and then give up.
Present bias: It is the tendency to choose a smaller gain in the present over a large gain in the future. It is related to the preference for immediate gratification. It is also known as hyperbolic discounting. Caregivers with such a bias might value present gratification more than greater benefits in the future—for example, reaping the benefits of micronutrients for children.
Behavioral Tools
Reminders: They can take many forms, such as an email, a text message, a letter, or an in-person visit reminding individuals of some aspect of their decision-making process. Reminders are designed to mitigate procrastination, oversight, and cognitive overload.
Intervention Design
Semi-structured interviews with caregivers were conducted in the catchment area of four SMI community-health teams in El Salvador. Interview designs were based on the existing literature pertaining to the non-adherence data and analyses of a household survey plus medical-record reviews of primary-care units from another study. In addition to the knowledge about context derived from previous field visits, these interviews explore bottlenecks in adhering to treatment. Health workers from each community health team selected the women to be interviewed after being provided with a few guideline characteristics regarding caregivers’ adherence to the treatment. A total of sixteen semi-structured interviews were conducted with women who had recently received the packets of micronutrients, along with instructions.
Based on the interviews, some trends emerged:
- Most nonadherence was related not to lack of attention, cognitive overload, or lack of information about treatment procedures. Rather, most mothers struggled with the “physical” barriers of treatment administration: the children did not like the taste, or the caregivers thought that certain undesirable symptoms in their child might be linked to the micronutrients (i.e., diarrhea, vomiting).
- Those small barriers sometimes prevented caregivers from providing their children with the micronutrients, but only when they saw no short-term benefits or an immediate need to administer the supplements (i.e., their child was not visibly unhealthy). If they did see improvements (in most cases, precisely because the child had been visibly unhealthy), they would find ways to overcome the child’s resistance.
- Most caregivers were not clear in their understanding of anemia and its consequences. The prevalence of anemia in the region is close to 50 percent, and the fact that most caregivers do not see it as a pressing health issue (even when advised by health workers) probably means that they underestimate the likelihood of their own children eventually acquiring the illness. They seemed to show concerns only when their children were diagnosed with anemia or when they perceived their children were unhealthy.
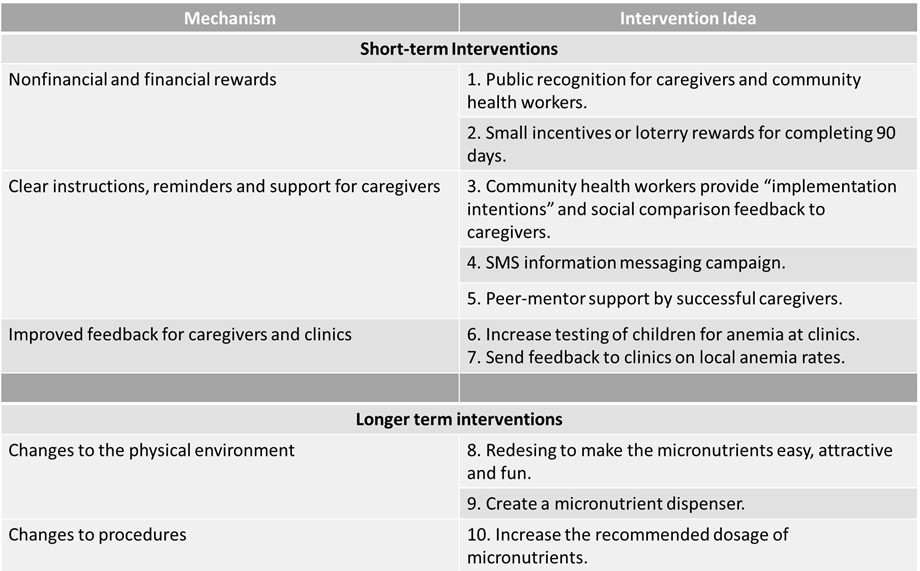
Using these insights, SMI considered ten different intervention options (see table 1), assessing them for impact and feasibility by calculating the cost to implement a given intervention. Three intervention ideas were then deemed feasible to implement and test: (1) an SMS information-messaging campaign, (2) peer-mentor support from successful caregivers, and (3) more well-visits testing for anemia in primary-care units .
Screening children for anemia in primary-care units was considered the intervention with the highest expected impact, although with low to medium scalability depending on available screening technology.
Table 1. Summary of Intervention Ideas
Results
With the redesigned intervention, the share of children receiving the full set of micronutrients increased to 82 percent, while the share of those adhering to treatment increased to 24 percent (a 9 percentage-point increase from baseline) (see figure 1).
Figure 1. Reception and Consumption of Micronutrients among Infants and Children Younger Than 24 Months (in percentages)
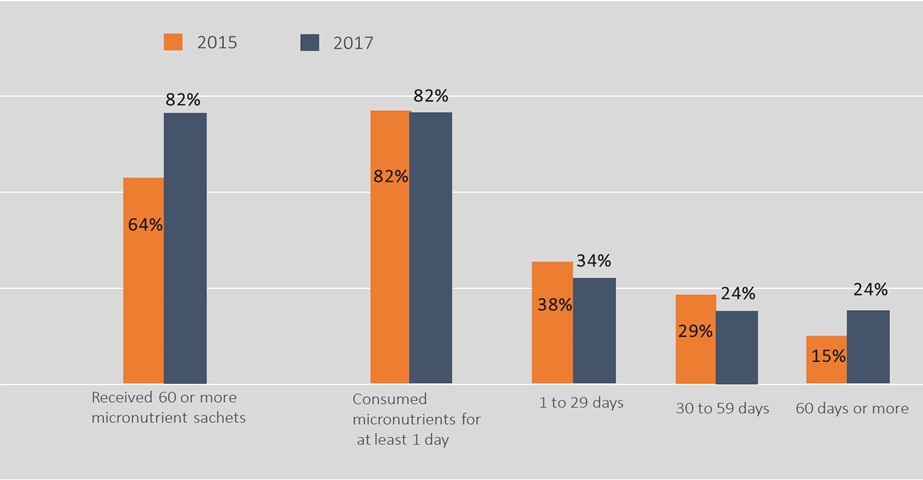
Despite the substantial progress, challenges remain on full adherence, as 76 percent of children still fell short of completing the total treatment, which is essential to reduce the prevalence of anemia.
Policy Implications
- The traditional approaches to public health issues for which there are clinically proven treatments are to focus, first, on distributing the treatment widely in the health systems, and, second, on developing communications campaigns to influence the knowledge and attitudes of both health workers and the population at risk regarding the benefits of the treatment. Both approaches are key building blocks for a solution, but they are not enough. Behavioral sciences can complement these approaches by focusing on key micro-decisions for takeup and designing the choice architecture leading to those decisions.
