Increasing the Use of Telemedicine

Context:
Argentina is one of the first adopters of telemedicine in the region. In 2019, 26% of hospitals nationwide reported offering telemedicine services to their patients. During the pandemic, the Argentinian telemedicine network experienced a rapid expansion within the private and public sectors, and regulations adapted to allow electronic or digital prescriptions, enabling their use in telecare platforms. The public platform TELESALUD hosted 120,000 consultations in 2020, a 600% increase from the previous year. In the same year, telemedicine demand for private health providers increased by 200%. Despite this unprecedented increase, telemedicine still occupies only a small place in the healthcare system.
Project:
To increase the take-up of telemedicine appointments, an informational campaign was created with the aim of reducing behavioral barriers to adoption. For the intervention, we partnered with APSOT, a health insurance company in Argentina, and Llamando al Doctor, the telemedicine company that provides telemedicine services to APSOT members and many others. For the intervention, about 3,500 households that had access to the system but had never used it were randomly allocated to a treatment and a control group. Households in the treatment arm received a series of messages that presented simple and actionable information about the benefits of telemedicine and how to use the service. The e-mails were sent from July 6 to August 24, 2021.
Behavioral Barriers:
Lack of information: People may lack relevant information, for instance, because information is difficult to obtain, scarce, or hard to understand. Patients may lack information and/or feel mistrust about the effectiveness of telemedicine. Individuals may not know how telemedicine works, and they may be worried that the quality of the physicians and the experience could be subpar.
Status Quo bias: Our tendency to maintain the current status of things. This current status, or status quo, is used as a reference point, and any change with regard to this point is seen as a loss. Telemedicine is an “experience good,” one that can be accurately evaluated and compared to its substitute (in this case, in-person visits) only after the product has been adopted and experienced. Hence, a change from in-person appointments to telemedicine may be perceived as a loss by the patient.
Hassle factors: We frequently do not act on our intentions because of small factors or inconveniences that hinder us or make us uncomfortable. Switching to telemedicine has some real—even if small—inconvenience factors, such as having to download and set up the technology, which could discourage its use, or trigger procrastination.
Present bias: The tendency to opt for a lesser benefit in the short term over a greater benefit in the longer term, which is associated with a preference for instant gratification. Due to present bias, individuals may not download the application, which makes people undervalue the future gains of having the service ready to use should they become sick.
Cognitive overload: The cognitive load is the amount of mental effort and memory used at a given moment in time. Overload is when the volume of information provided exceeds an individual’s capacity to process it. Once patients are sick, the cognitive burden could be too high for individuals to use telemedicine services for the first time.
Optimism bias: Optimism bias makes us underestimate the probability of negative events and overestimate the probability of positive events. Optimism bias could lead people to underestimate the probability of getting sick, making it less likely that they will download the app and register for telemedicine options.
Loss aversion: Refers to the idea that a loss causes distress that is greater than the happiness caused by a gain of the same size, when two options that involve risk and uncertainty are relatively compared. This is why we are more willing to take risks to avoid a loss. Thus, loss aversion could cause people to think that using telemedicine could jeopardize access to in-person visits later on.
Mistrust: Patients underestimate or mistrust the quality of care an app could provide and the app’s ability to manage any queries during a virtual medical appointment. To reduce mistrust, the e-mails sent to the treatment groups also highlight that the service is provided by the same doctors whom patients see during their in-person visits.
Behavioral Tools:
Reminder: Reminders may consist of an email, text messages, a letter, or a personal visit to remind the person making the decision about some aspect of their intention-action. These are aimed at mitigating procrastination, forgetfulness, and cognitive overload for those who must make decisions. Reminders, messages, and other behaviorally informed treatments are used in this study to encourage and guide users toward telemedicine appointments.
Simplification: Reducing the effort required to perform an action by making the message clearer, cutting the number of steps, or breaking down a complex goal into simple, easier steps. The messages in the treatment groups present simplified access to information about the benefits of Llamando al Doctor and easy-to-follow guides for using the service.
Planning tools: Messages designed to encourage individuals to make a concrete plan for taking action. They urge the individual to divide the objective (for example, going to a medical appointment) into a series of smaller, concrete tasks (leaving work early, finding a babysitter, postponing a weekly meeting, etc.). These often include a space for writing down crucial information such as the date, time, and place.
Intention-action gap: Refers to the idea that people do not always do the things that they intend to do. Factors that often explain the gap are procrastination, missed opportunities, doubts, emotionally charged situations, difficulty of the task, and a lack of clear steps to move forward. In the context of this informational campaign, the messages include actionable steps on how to download the app and calls to action.
Salience: Our attention is limited. Therefore, behavioral economics pays special attention to the moment when a message is delivered, the location in which is delivered, and the content it emphasizes. For instance, by underlining or writing in bold keywords or phrases in the emails, users are guided more easily toward the steps required for telemedicine alternatives.
Priming: Priming is a phenomenon in which exposure to one stimulus influences how a person responds to a subsequent stimulus. These stimuli are often conceptually related words or images. The treatment group messages also contain priming questions designed for the reader to actively consider their choice of using telemedicine.
Personalization: Personalizing information based on individual characteristics and traits of identity is shown to improve responsiveness and outcomes. By providing quotes and the personal information of the doctors, the messages generate personalization and familiarity.
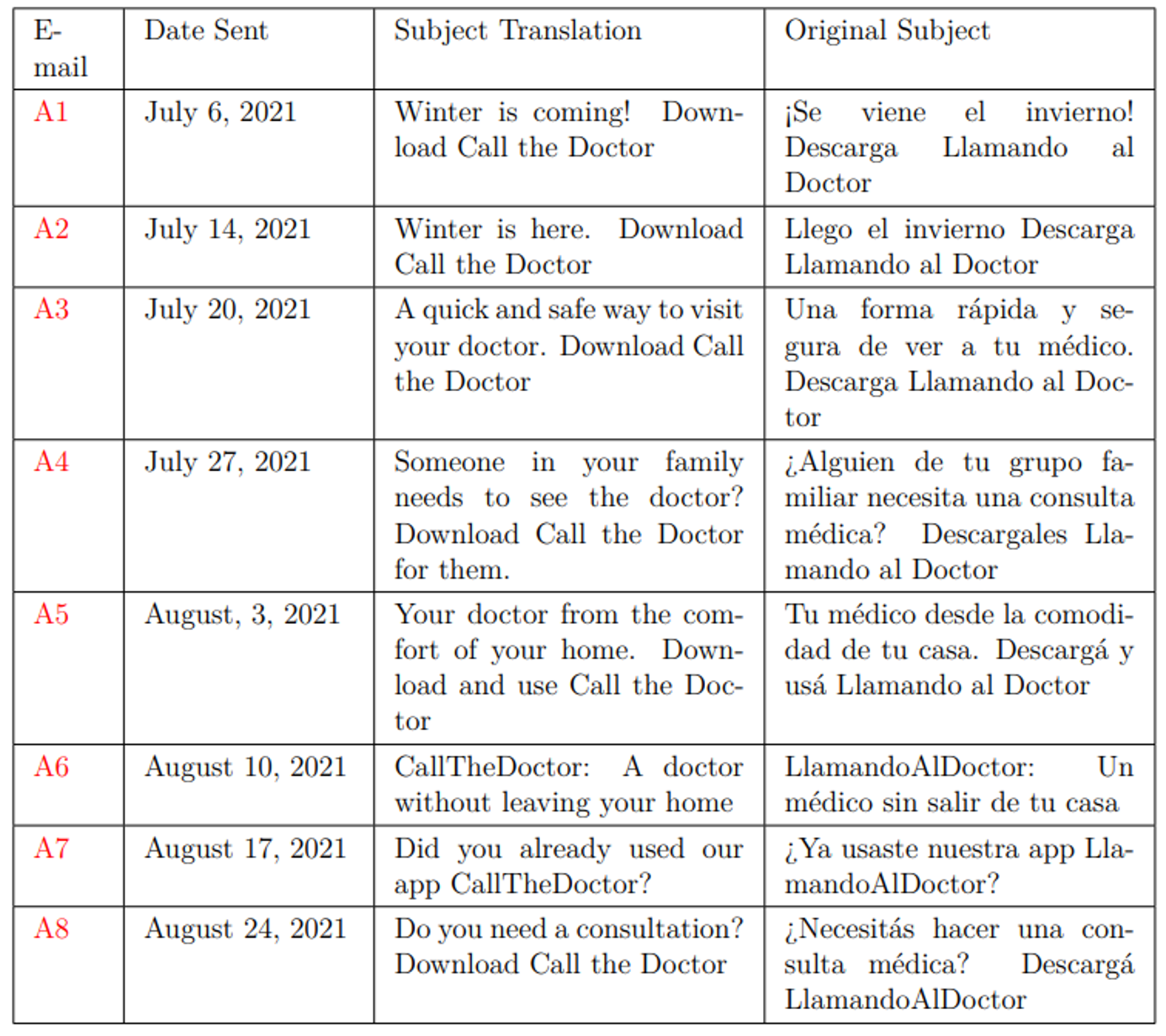
For this study, we conducted a communication campaign in partnership with APSOT, a private health insurance company that serves the managerial staff of the Techint Group in Argentina. A sample of 3,548 households was randomized into a control and a treatment group (1,774 in each group.) Two strata were used during the randomization: households that live in the capital city of Argentina (29%) and those that live in other cities (71%). The intervention consisted of eight e-mails sent by APSOT between June 6 and August 24, 2021. Table 1 presents the dates and subject lines of these e-mails.
Table 1: E-mail campaign Timeline
First, we conducted an event study approach to evaluate the differences in downloads of the application during each week of 2021. Then, we measured the intent to treat effect of the communication campaign, i.e., whether there exist changes in the probability that a household in the treatment group would have used the service compared to one in the control group. Additionally, to compute the effect of the e-mails for those who actually opened them, we ran an instrumental variable model of the variable Read that indicates which households opened at least one e-mail using assignment to treatment T as the instrument.
- The sample is relatively small and not representative of the overall population of Argentina.
- We could not link the downloads to each individual member, so we can only present suggestive evidence on the number of households downloading the mobile application, which is a prerequisite to being able to use telemedicine services when needed.
- Unfortunately, only about 50% of the households in the treatment opened the e-mail.
- Even though we partnered with a health insurance company, we cannot estimate the impact of using telemedicine on in-person visits and health outcomes. For example, is telemedicine a substitute or complement to in-person visits? Does it improve health outcomes by providing more and easier access to doctors?
- Future research may need to pair the take-up intervention with a full evaluation of the long-term impact on those outcomes.
Results:
This paper shows that information campaigns can be successful in increasing telemedicine use.
- The number of e-mails read weekly ranged from 435 to 613, with a decreasing trend over time. By the end of the campaign, 901 households, or 51% of the treatment sample, had opened at least one of the e-mails.
- The application download growth relative to the baseline is statistically significant for the first three weeks after the first intervention, with user growth also significant at week 5.
Five months after the beginning of the campaign, the treatment group was 4.1 pp more likely to have used telemedicine compared to the control group. The difference between the treatment and control groups grew over time to 4.5 pp after six months and to 6 pp after eight months. This is about three-and-a-half times larger.
Figure 1: Cumulative Calls and First-Time telemedicine Users
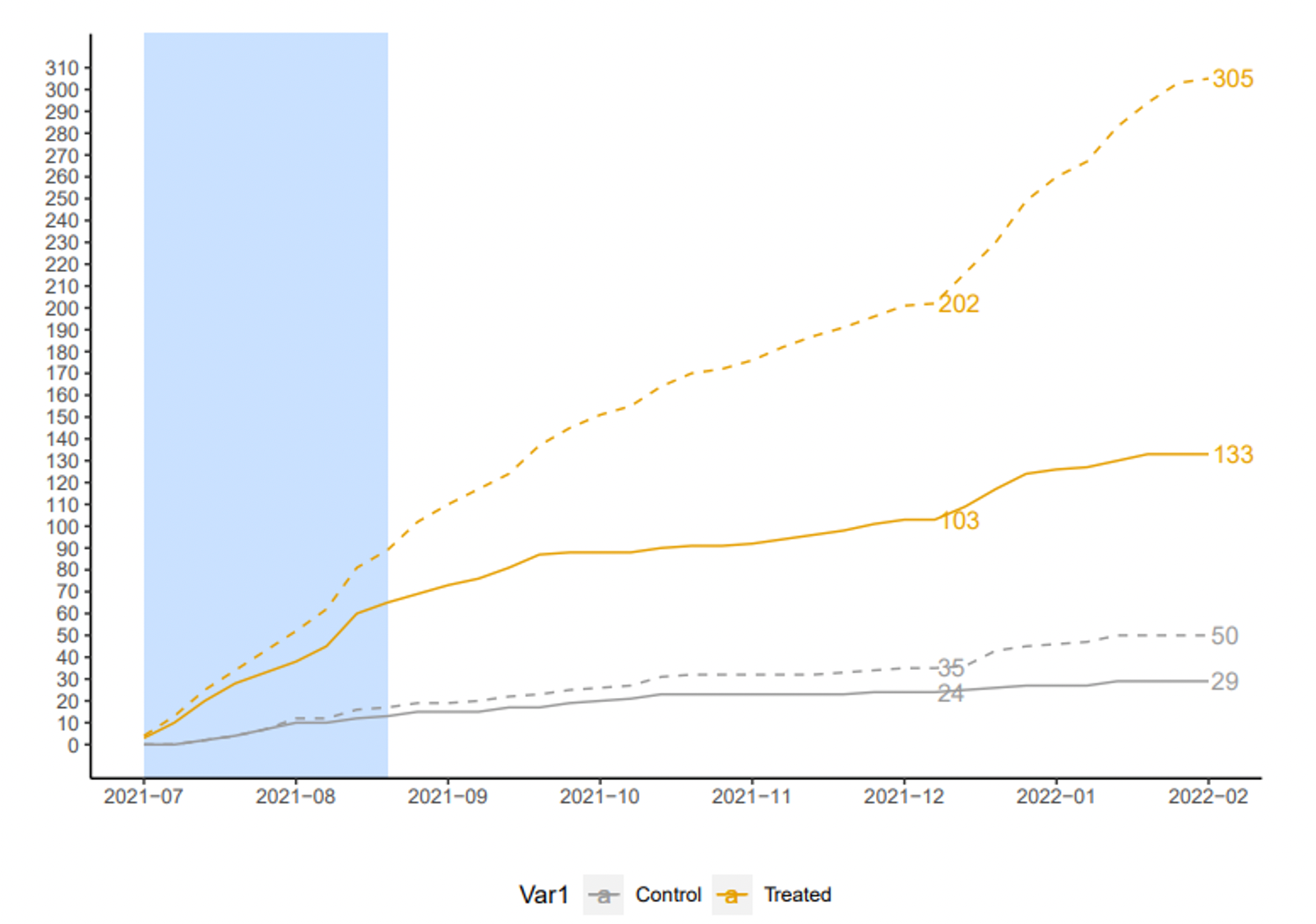
Note: This figure shows the number of cumulative calls and new users of the mobile application by control
and treatment group. The yellow lines represent the demand growth of the treatment group, the dashed
line indicates number of calls, and the solid line indicates number of first-time users. Similarly, the gray
lines represent the demand of the control group, with the dashed line indicating the number of calls and
the solid line indicating the cumulative number of first-time users. The light blue panel indicates the
period of the communication campaign.
- As expected, given the opening rate of e-mails, the results of the instrumental variable model are now twice as large. For the individuals who opened at least one e-mail, the probabilities of having used the service were 8.1 pp, 9 pp, and 11.9 pp larger than for those in the control group at each data cut-off.
- By the end of 2021, the treatment group had 103 new first-time users compared to 24 in the control group. By the eighth month, the difference was 133 to 29, more than four-and-a-half times larger.
- As expected, the number of total calls grows even more than first use for both treatment and control groups. By the last cut-off date, the average user in the treatment group had made more than two calls--six times more than the average user in the control group.
Policy Implications:
- Reminders, messages, and other behaviorally informed treatments can be used to increase compliance in the health sector. In the context of this study, messages that employ digital tools and tackle behavioral barriers changed the behavior of patients as seen by an increase in the use of telemedicine.
- The results of this paper highlight that the demand for “experience goods,” such as telemedicine, changes significantly after individuals try them for the first time. This finding further shows that regulation could play a role in increasing the use of a service that is under-consumed in the market, and that could hugely benefit individuals at a very low cost.
- Making telemedicine mandatory at the health insurance level risks exit to other insurers, while making it mandatory at the national level could generate political backlash. Behaviorally informed interventions, such as those described in this paper, are less controversial and can easily complement the set of policy tools for experience goods.
- Well-implemented, behaviorally informed treatments, such as the one presented in this study, could help in lowering costs and decreasing inequality in access to healthcare, especially when there exist mobility restrictions.
