Reducing Behavioral Barriers to Telemedicine Use

Context
The consolidation of mobile telephony is revolutionizing communication and the way people access services. The mobile phone revolution offers an unprecedented opportunity for the provision of healthcare consultation and services where and when people need it. Telemedicine applications (apps) are harnessing this opportunity to improve patient outcomes by optimizing care, saving time and cost, and expanding access to healthcare services and medical information.
Llamando al Doctor is a video-call medical service available on a digital app that users can download to their mobile phones. The video-call service is available 24 hours a day, every day, and connects users (i.e., patients) directly with qualified doctors. Llamando al Doctor establishes agreements with health-service providers in Argentina that offer the service to their affiliates as part of their coverage plans.
The Project
Llamando al Doctor, a private Argentine healthcare provider, and the IDB Behavioral Economics Group carried out a study to understand the impact of telemedicine on the health consumption of users. The study first sought to analyze the effectiveness of different communication methods to promote registration for the app by sending email and mobile phone text messages that detailed its benefits and attributes. The second stage meant to study of the app’s effects on the volume and type of consumption of face-to-face patient–to–health professional consultations.
Behavioral Analysis
Behavioral Barriers
Status quo bias: It is the tendency of citizens to maintain the current state of affairs, even when change is clearly better. This current status, or status quo, is used as a reference point, and any change with regard to this point is seen as a loss. Patients are used to face-to-face consultations with their trusted doctor.
Lack of information, disinformation: Patients don’t know about the app, and if they do, they do not understand how the app works in terms of cost and availability of doctors.
Other Barriers
Mistrust: Mistrust occurs when one party is unwilling to rely on the actions of another party in a future situation. Patients underestimate or distrust the quality of care an app can provide and the app’s ability to manage any queries during a virtual medical appointment.
Behavioral Tools
Reminders: They can take many forms, such as an email, a text message, a letter, or an in-person visit reminding individuals of some aspect of their healthcare decision-making process. Reminders are designed to mitigate procrastination, oversight, and cognitive overload.
Loss aversion: It is the idea that losses cause a distress that exceeds the happiness brought by a gain of the same size. The threat of loss can trigger an aversion that can be leveraged to nudge behaviors in a positive direction.
Prominence: Human beings have limited stores of attention. Making key elements visible and prominent at the proper time and place is as important as the message itself.
Simplification: Reducing the effort required to perform an action. For example, cutting the number of steps involved in achieving a complex goal, or break it down into simpler steps.
Social norms: These are the unwritten rules that govern behavior within a society.
Group identity: People have an innate sense of belonging. They have the need to belong to groups they identify with.
Intervention Design
Health provider administrative records (sociodemographic characteristics, consumption of healthcare services, app downloads, and registrations) were used to randomize over 22,700 affiliates into treatment and control groups, which were sorted into sixteen strata.
Messages were designed to target affiliates in the treatment group. In total, six messages were sent between July and October 2019: three emails and three text messages. The six messages were split into three pairs of messages, each comprising an SMS and an email, separated by a week’s time.
Timeline
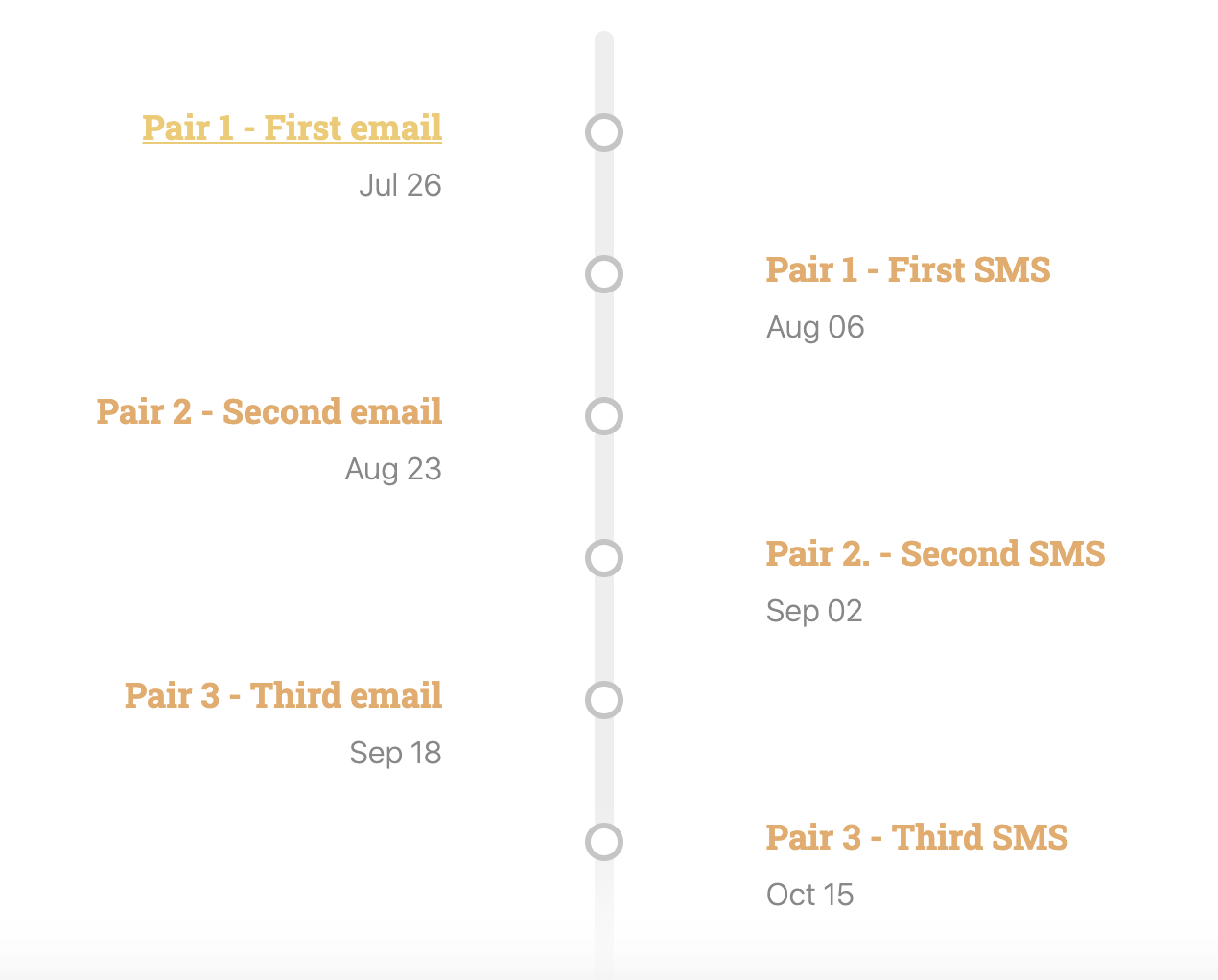
The messages were sent by the health providers’ automated message management system using their contact information database of affiliates (email and telephone).
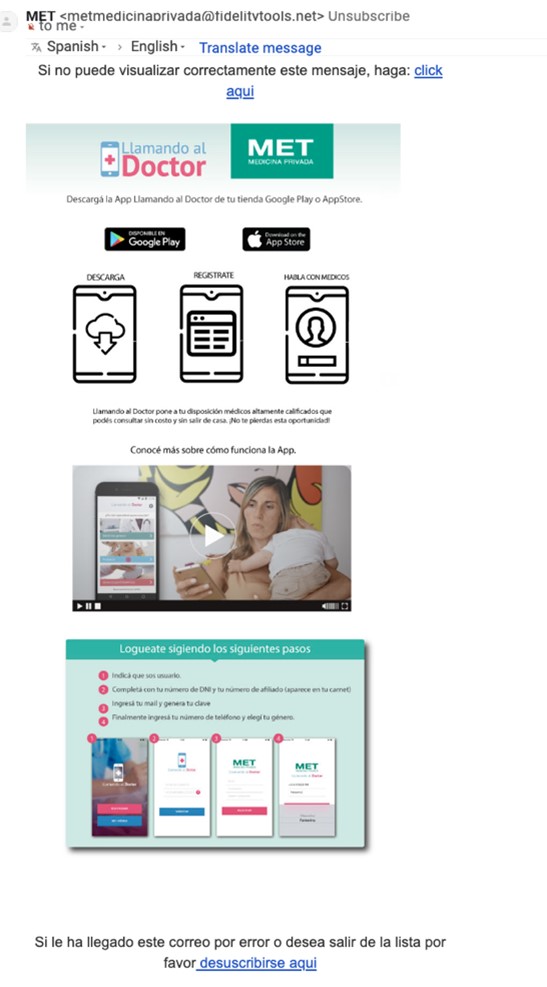
Example of Email Designed for Treatment Group
Challenges
Implementation error: Although affiliates were randomly assigned to a treatment group and a control group, the automated message management system sent the messages to the entire sample and not to the subset of affiliates assigned to the treatment group.
Results
Implementation error: Although affiliates were randomized to a treatment group and a control group, the automated message management system sent the messages to the entire sample and not to the subset of affiliates assigned to the treatment group.
This resulted in all affiliates receiving the treatment (six messages), which precluded a rigorous effectiveness analysis. It also prevented a second-stage evaluation of the effect of this telemedicine technology on health consumption indicators.
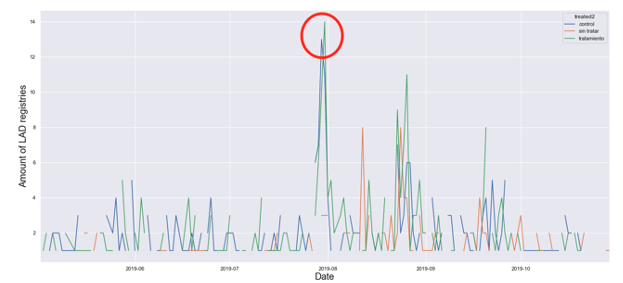
A simpler observation of registrations trends with the app within the sample shows a positive correlation between the treatment (messages) and registrations. Figure 1 presents the total number of new registrations between June 2018 until October 2019 (dates of intervention are July 26 to October 15). Figure 2 disaggregates registrations by treatment and control groups. It shows that new registrations peak on the days when treatments are implemented.
Figure 1. New Registrations between June 2018 and October 2019
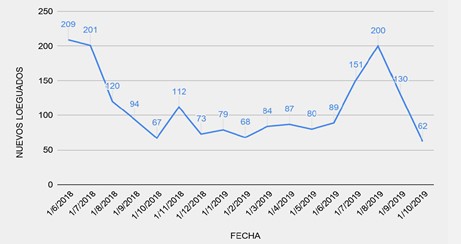
Figure 2. Registrations by Treatment and Control Groups
Policy Implications
- Mobile technologies for health services are an attractive tool for health providers in the region. Even though we couldn’t fully test it in this project, behavioral insights can help promote their use through nudges that reduce behavioral barriers to entry. For instance, they can help people overcome biases such as status quo and barriers like mistrust for remote connection to doctors and uncertainty regarding the quality of the services provided.
- Health providers can also design cost-effective campaigns to reduce the gap in information regarding the benefits of telemedicine. Increased use of remote health services can extend access to patients, reduce the time they spend travelling to hospitals while they accrue efficiency gains for resource management and costs among health providers. The Llamando al Doctor pilot in Argentina provides a complete roadmap for interested parties in the health and telemedicine sector to implement agile, cost-effective, and collaborative interventions to promote use of telemedicine in Argentina.
- Our descriptive results showing increasing numbers of daily registrations to Llamando al Doctor following the email and SMS campaigns show promising prospects for telemedicine in Argentina and the region.
